
Boire’s lab in the Human Oncology and Pathogenesis Program and the paper’s other first author, led the analysis of the fluid.

Back to top Using Science to Ask Clinical Questions At that point, the rest of the fluid was taken to the lab of MSK physician-scientist Adrienne Boire for further study. Thirteen of the 18 patients had spinal taps to look for the virus, but it was not found. MSK’s microbiology team devised a test to detect the COVID-19 virus in the fluid.

When nothing was found in the scans that would explain their condition, the researchers thought the answer might lie in the cerebrospinal fluid.
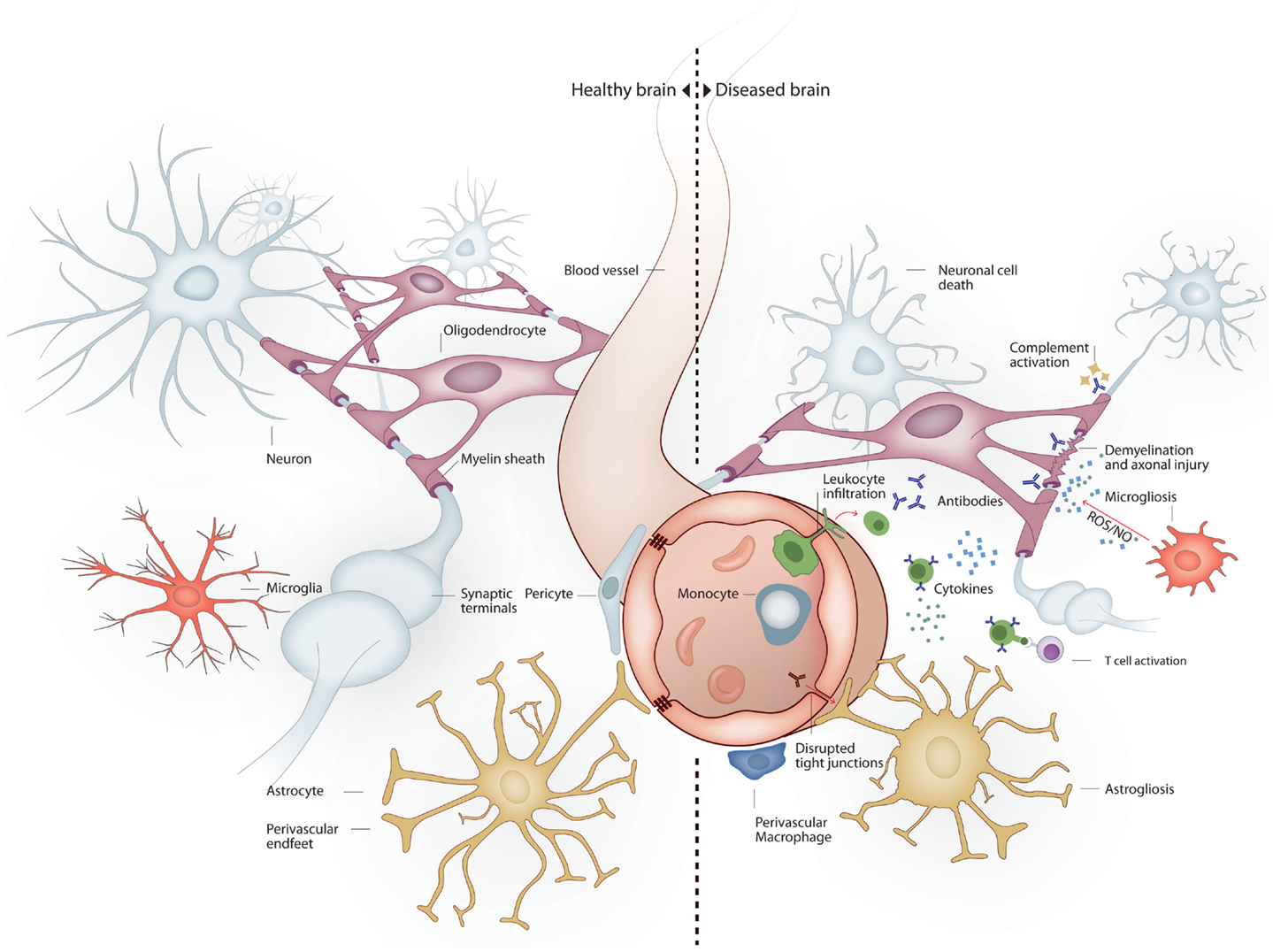
Inflammation of the brain full#
The patients were given a full neurology workup, including brain scans like MRIs and CTs and electroencephalogram (EEG) monitoring, to try to find the cause of their delirium. The study in the Cancer Cell paper focused on 18 patients who were hospitalized at MSK with COVID-19 and were experiencing severe neurologic problems. They first suspected that the virus itself was having an effect on the brain. When the MSK team first began studying COVID brain, though, they didn’t know that cytokines were the cause. But cytokines can seep into the area around the brain and cause inflammation. When CAR T cell therapy is given, it causes immune cells to release molecules called cytokines, which help the body to kill the cancer. It is a side effect in patients who are receiving a type of immunotherapy called chimeric antibody receptor (CAR) T cell therapy, a treatment for blood cancer. Wilcox says, because they are already used to treating the condition in other systemic inflammatory syndromes. Members of MSK’s Department of Neurology felt well-poised to study it, Dr. The medical term for COVID brain is encephalopathy. Learn more Recognizing a Familiar Symptom “That meeting turned into a tremendous collaboration between neurology, critical care, microbiology, and neuroradiology to learn what was going on and to see how we could better help our patients.” “We were initially approached by our colleagues in critical care medicine who had observed severe delirium in many patients who were hospitalized with COVID-19,” says Jessica Wilcox, the Chief Fellow in neuro-oncology at MSK and one of the first authors of the new study. The findings suggest that anti-inflammatory drugs, such as steroids, may be useful for treating the condition, but more research is needed. In the February 8, 2021, issue of the journal Cancer Cell, a multidisciplinary team from Memorial Sloan Kettering reports an underlying cause of COVID brain: the presence of inflammatory molecules in the liquid surrounding the brain and spinal cord (called the cerebrospinal fluid). It usually emerges weeks after someone first becomes sick with COVID-19.

In severe cases, it can lead to psychosis and even seizures. One of the dozens of unusual symptoms that have emerged in COVID-19 patients is a condition that’s informally called “COVID brain” or “brain fog.” It’s characterized by confusion, headaches, and loss of short-term memory. Find a Researcher Programs & Centers Postdoctoral Positions Research TopicsĪ unique collaboration among experts from several areas within MSK leads to findings about how inflammation appears to be driving the neurologic effects seen in some COVID-19 patients.Gerstner Sloan Kettering Graduate School of Biomedical Sciences.Find a Doctor Refer a Patient Newsletter Sign Up Clinical Trials.Anesthesiology & Critical Care Medicine.Find a Doctor Make an Appointment Visitor Information FAQ.Find a Doctor Make an Appointment Visitor Information MyMSK.


 0 kommentar(er)
0 kommentar(er)
